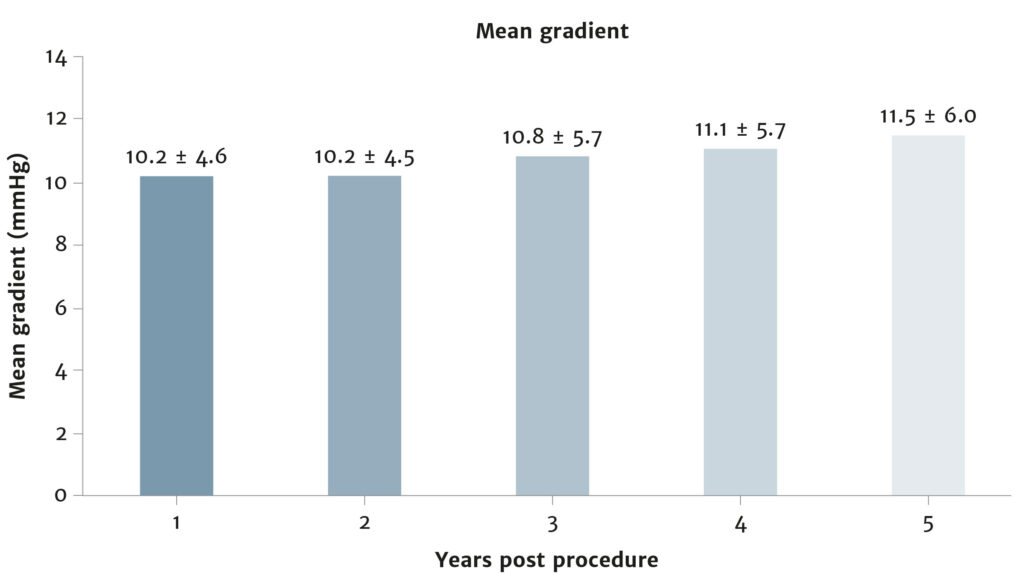
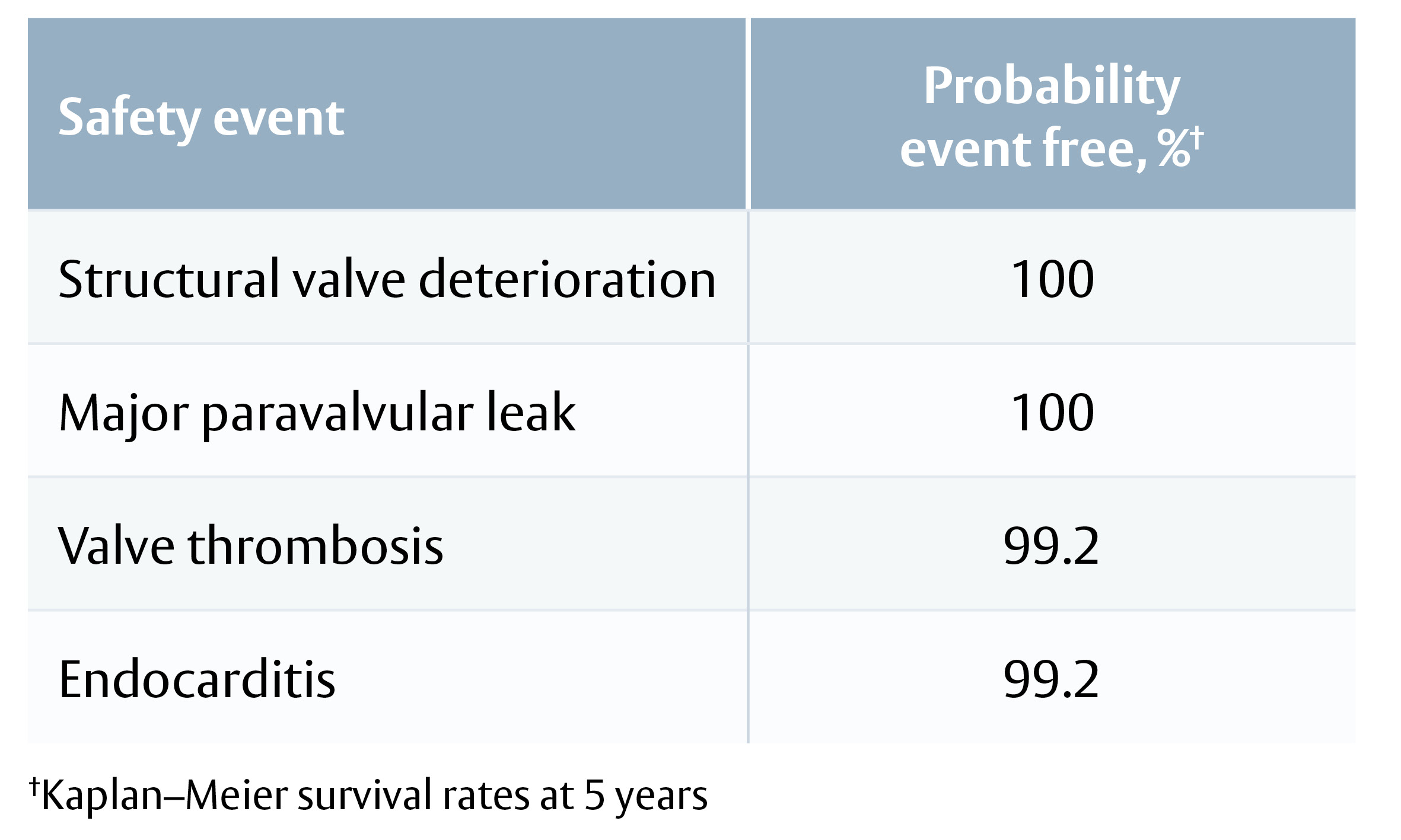
At 5 years, COMMENCE results indicate a favourable safety profile and stable haemodynamic performance of a bioprosthetic valve with RESILIA tissue. Ten-year data in an extended follow-up cohort and the RESILIENCE trial with 11-year follow-up are forthcoming.
Single center experience with INSPIRIS RESILIA aortic valve
Prof. D’Onofrio – EACTS 2021
Prof. Kocher – EACTS 2021
Prof. Hanneke Takkenberg – EACTS 2021
Edwards Lifesciences Symposium
Prof. Hanneke Takkenberg
Be courageous, be experienced, be ethical … according to the Guidelines!
Prof. Bart Meuris
Be courageous, be experienced, be ethical … according to the Guidelines!
Prof. Michael Borger
Be courageous, be experienced, be ethical … according to the Guidelines!
Ai L et al. Innovations. 2017; 12: 338–45. DOI: 10.1097/imi.0000000000000407
Aim
To develop a clinically relevant aortic root model, and then compare the haemodynamic function of the EDWARDS INTUITY valve (a rapid deployment valve) with the Carpentier- Edwards PERIMOUNT Magna Ease valve (a conventional bioprosthetic valve), in vitro.
Background Information
Many trials have shown the short-term safety and efficacy of sutureless rapid deployment aortic valves, but direct comparisons of the haemodynamic performance of these new valves with conventional bioprosthetic valves are lacking.
Methods
Model development
Multi-slice computed tomography reconstructions in patients with aortic stenosis were used to generate a 3D printed model of an aortic root.
Effective diameter of the aortic annulus was 21 mm, effective area was 3.38 cm2 and LVOT area was 3.01 cm2.
Valve Deployment
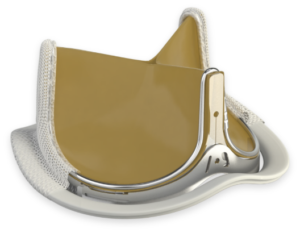
For measurement of haemodynamic parameters (EOA, TPG and LVOT geometry), Magna Ease valves were sutured to the model’s annulus, with and without the use of pledgets, and EDWARDS INTUITY valves were secured by balloon inflation. EDWARDS INTUITY
valves were further tested with frames expanded
to 22, 23, 24 and 25 mm.
Figure 1: EDWARDS INTUITY and Magna Ease valves in the aortic root model and cadaver heart
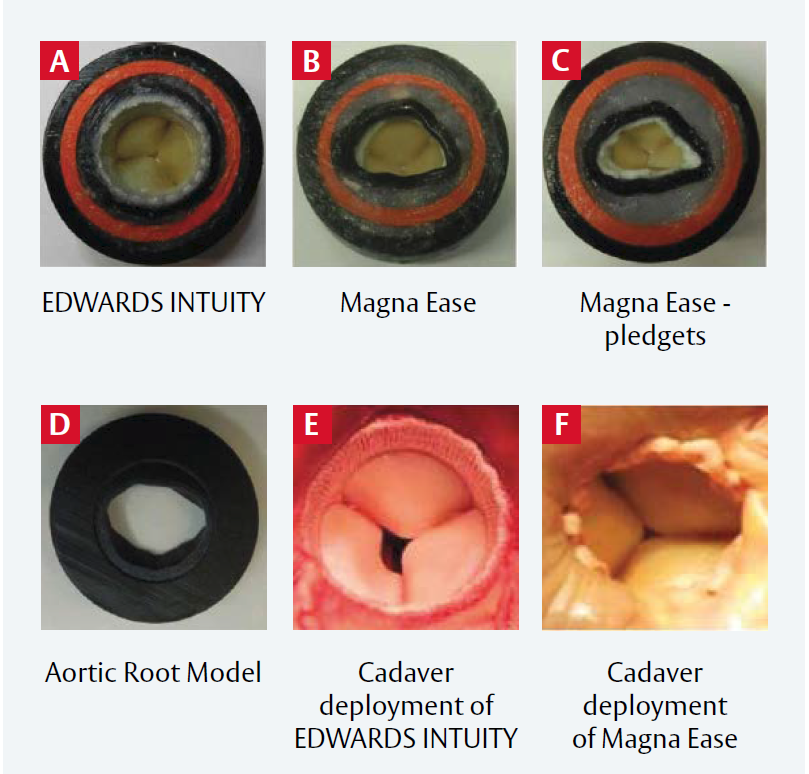
A: EDWARDS INTUITY valve in the model;
B: Magna Ease valve in the model without pledgets;
C: Magna Ease valve in the model, with pledgets;
D: Outflow view of the aortic root model; E: EDWARDS INTUITY valve in the cadaver heart;
F: Magna Ease valve without pledgets in the cadaver heart.
Reproduced from Ai L et al, 2017. © 2017 Wolters Kluwer Health, Inc. Reproduced with permission LVOT in the rubber gasket aortic root model and in the cadaver heart.
Results
Hemodynamic Performance
The EDWARDS INTUITY valve had both a greater EOA and a lower TPG than the Magna Ease valve, irrespective of pledget use (Figure 1). EOA
and TPG were also significantly different between Magna Ease valves with and without pledgets (all p<0.002 or 0.001).
LVOT Performance
Expanding the EDWARDS INTUITY valve frame diameter from 22 to 25 mm increased the average LVOT area index stepwise from 1.07 to 1.34: this minimally affected EOA or TPG (Table 1).
EDWARDS INTUITY valves resulted in more circular LVOTs than Magna Ease valves, although increasing ellipticity did not impact EOA or TPG.
Average maximum flow velocity was lower across the EDWARDS INTUITY valve than the Magna Ease valve without pledgets (p<0.003), as were maximum turbulent shear stress (p<0.02) and turbulent kinetic
energy (p<0.002).
| EDWARDS INTUITY valve (n=4) | Magna Ease valve (n=4) | Magna Ease valve with pledgets (n=4) | |
| EOA, cm2 | 1.85 ± 0.06 | 1.56 ± 0.01 | 1.21 ± 0.08 |
| Mean gradient, mmHg | 16.8 ± 1.3 | 23.4 ± 0.51 | 1.21 ± 0.08 |
EOA: effective orifice area
Table 1: TPG and EOA of models with an EDWARDS INTUITY valve or a Magna Ease valve (with or without pledgets)
Limitations
- Such a model, isolated from the left ventricle, cannot replicate all physiological mechanical properties.
- Pathological changes and normal physiological variations can affect valve performance in vivo: these were not modelled here.
- The use of saline, rather than blood or a substitute, may have affected simulated valve performance.
Conclusions
- Haemodynamic performance was superior for the EDWARDS INTUITY valve than the Magna Ease valve with increased EOA and reduced mean gradient.
- Pledgets worsened Magna Ease valve performance.
- Maximum velocity, turbulent shear stress and kinetic energy were all lower across the EDWARDS INTUITY valve than the Magna Ease valve.
- Haemodynamic advantages may account for the superior clinical performance of rapid deployment valves over conventional surgical valves
Important safety information:
Use of the EDWARDS INTUITY Elite valve system may be associated with new or worsened conduction disturbances,
which may require a permanent cardiac pacemaker implant (PPI). The rate of PPI for the EDWARDS INTUITY Elite
valve is within the range reported in the literature for various rapid deployment valves, but higher than that reported
for surgical aortic valves. Physicians should assess the benefits and risks of the EDWARDS INTUITY Elite valve prior to
implantation. See instructions for use for additional information.
For professional use. For a listing of indications, contraindications, precautions, warnings, and potential adverse events, please refer to the Instructions for Use (consult eifu.edwards.com where applicable).
Edwards devices placed on the European market meeting the essential requirements referred to in Article 3 of the Medical Device Directive 93/42/EEC bear the CE marking of conformity
Edwards, Edwards Lifesciences, the stylized E logo, Carpentier-Edwards, Carpentier-Edwards PERIMOUNT, EDWARDS INTUITY, EDWARDS INTUITY Elite, Magna, Magna Ease, PERI, PERIMOUNT and PERIMOUNT Magna are trademarks are trademarks or service marks of Edwards Lifesciences Corporation or its affiliates. All other trademarks are the property of their respective owners.
© 2021 Edwards Lifesciences Corporation. All rights reserved. PP–EU-2350 v1.0
Edwards Lifesciences • Route de l’Etraz 70, 1260 Nyon, Switzerland • edwards.com
Rodríguez-Caulo, Emiliano A., et al., Journal of Thoracic and Cardiovascular Surgery (2021) DOI:10.1016/j.jtcvs.2021.01.118
Aim
Evaluate long-term survival and major adverse events in patients aged 50 to 65 years with a primary isolated AVR, with a bioprosthesis or mechanical valve, because of severe AS
Methods
- National observational study with all consecutive patients aged 50-65 who underwent AVR because of severe isolated AS between 2000 and 2018 in 27 hospitals in Spain
- In total, 5215 patients were included in the study (21% were bioprostheses)
- Among bioprostheses, 46.8% were Carpentier-Edwards, 19.4% Mitroflow, 4.2% Mosaic and 4.1% Trifecta
- 2:1 propensity matching analysis (1822 Mech and 911 Bio) with a mean follow-up of 8.1 years
Results
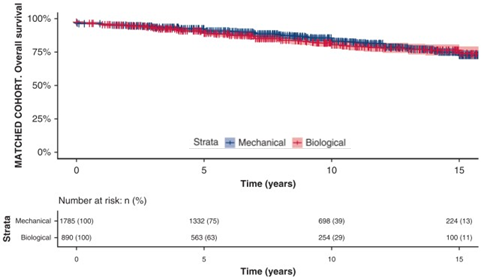
- In the matched cohort, long-term survival differences were not observed (cf. figure)
- Overall survival after Mech valves at 5, 10, 15 and 18 years of follow-up were 91%, 83%, 73% and 62% vs. 89%, 81%, 74% and 72% for bioprostheses, respectively
- Minor differences in survival were found in patients aged 50-55 years (P = 0.11)
- No significant differences in the composite of stroke, bleeding and reintervention (P = 0.484)
- Major bleeding (P = 0.002) and strokes (P = 0.095) had a higher frequency in the Mech valve group
- Rates of reoperation were significantly higher in the bioprosthesis valve group (P < 0.001)
- In a 1:1 propensity matching, the risk of reintervention in the Bio group decreased for patients who underwent AVR between 2009 and 2018 compared with 2000 to 2008
Conclusions
- Bioprostheses seem a reasonable choice for patients aged 50 to 65 years in Spain, particularly for those older than 55 years, because of the long-term survival and the lower-risk related, especially, to major bleeding compared with mechanical prostheses
- However, the higher risk of reoperation with bioprostheses should be considered and discussed with the patient to make the best-informed decision
Key talking points
Are these outcomes aligned with guideline recommendations? – Current ESC/EACTS guidelines consider mechanical and bioprosthetic valves as reasonable in patients aged 60 to 65 years, whereas AHA/ACC guidelines consider both reasonable in 50 to 65 y.o. patients. Therefore, findings from this national observational study with patients that underwent isolated AVR seem to be more aligned with the latest American guidelines.
Why did the risk of reintervention decrease in patients who underwent Bio AVR between 2009 and 2018? – The authors point to improved outcomes after AVR for both mech and bio prostheses after 2009. In the unadjusted cohort, there was a significant decrease in stroke, major bleeding and reintervention. In the bio group, the rate of reoperation because of SVD diminished from 7.6% to 4% after 2009, which is related to the durability of bioprostheses. Improvements in the bio group may be linked to the incorporation of newer anticalcification properties.
What is the mortality risk associated with prosthesis reintervention? – Today, mortality risk associated with prosthesis reintervention has been minimized, and most recent bioprostheses allow for “valve-in-valve” procedures for patients at high surgical risk.
For professional use. For a listing of indications, contraindications, precautions, warnings, and potential adverse events, please refer to the Instructions for Use (consult eifu.edwards.com where applicable).
Edwards devices placed on the European market meeting the essential requirements referred to in Article 3 of the Medical Device Directive 93/42/EEC bear the CE marking of conformity
Edwards, Edwards Lifesciences, the stylized E logo, Carpentier-Edwards are trademarks or service marks of Edwards Lifesciences Corporation or its affiliates. All other trademarks are the property of their respective owners.
© 2021 Edwards Lifesciences Corporation. All rights reserved. PP–EU-2029 V1.0
Edwards Lifesciences • Route de l’Etraz 70, 1260 Nyon, Switzerland • edwards.com
Dr. Bart Meuris, Belgium
Keywords: aortic root replacement; aortic stenosis; aortic valve replacement; Bentall; Valsalva graft
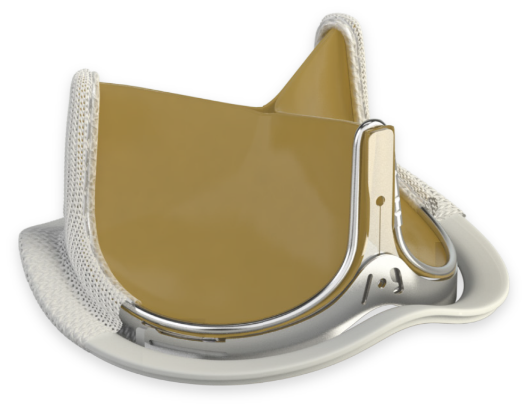
Although the majority of Bentall procedures have been performed with mechanical valves, the use of bioprosthetic valves is increasing. Modifications to the Bentall procedure may further enable the use of bioprosthetic valves: use of Valsalva pseudosinuses may reduce stress on the bioprosthetic leaflets and reduce the incidence of thromboembolism.
Chirichilli et al. routinely perform the Bentall procedure using the Valsalva graft with a Carpentier‑Edwards PERIMOUNT or PERIMOUNT Magna Ease valve. Here, they present the long‑term follow-up data assessing durability and valve-related complications.
Click on the link below to find out more about the performance of the PERIMOUNT valves combined with a modified Bentall procedure.
Click here to access the full publication
For professional use. For a listing of indications, contraindications, precautions, warnings, and potential adverse events, please refer to the Instructions for Use (consult eifu.edwards.com where applicable).
Edwards devices placed on the European market meeting the essential requirements referred to in Article 3 of the Medical Device Directive 93/42/EEC bear the CE marking of conformity.
Edwards, Edwards Lifesciences, the stylized E logo, Carpentier-Edwards, Magna, Magna Ease, PERI, PERIMOUNT and PERIMOUNT Magna are trademarks or service marks of Edwards Lifesciences Corporation or its affiliates. All other trademarks are the property of their respective owners.
© 2020 Edwards Lifesciences Corporation. All rights reserved.
Edwards Lifesciences • Route de l’Etraz 70, 1260 Nyon, Switzerland • edwards.com
Keywords: aortic bioprostheses; aortic stenosis; aortic valve replacement
Surgical aortic valve replacement (SAVR) is still offered to elderly populations despite the potential for structural valve degeneration. Currently, however, there is limited comparative data on the long-term durability of different SAVR prostheses.
Reporting outcomes including repeat aortic valve replacement, prosthetic valve endocarditis and late all-cause mortality, Biancari et al. present key results from a retrospective, non-randomised, propensity-matched comparative analysis of the Trifecta and Carpentier-Edwards PERIMOUNT Magna Ease valves. The authors compared the outcomes of 2,216 patients who had undergone the procedure to implant one of the two SAVR prostheses.
Click the link below for an update on the latest research in aortic valve replacement.
Click here to access the full publication
For professional use. For a listing of indications, contraindications, precautions, warnings, and potential adverse events, please refer to the Instructions for Use (consult eifu.edwards.com where applicable).
Edwards devices placed on the European market meeting the essential requirements referred to in Article 3 of the Medical Device Directive 93/42/EEC bear the CE marking of conformity.
Edwards, Edwards Lifesciences, the stylized E logo, Carpentier-Edwards, Magna, Magna Ease, PERI, PERIMOUNT and PERIMOUNT Magna are trademarks of Edwards Lifesciences Corporation or its affiliates. All other trademarks or service marks are the property of their respective owners.
Keywords: aortic valve replacement; pericardial bioprostheses; reintervention
The use of pericardial bioprostheses in aortic valve replacement (AVR) is highly popular due to the lack of need for lifelong anticoagulation. Despite this, few studies have investigated the durability, rates of structural valve degeneration and valve-related events in newer bioprostheses.
In this article Lam et al. present key results from a single-centre, retrospective study comparing three different aortic bioprosthetic valves . The authors assessed rates and causes of reinterventions in patients who underwent AVR with the Trifecta, Mitroflow and Carpentier-Edwards PERIMOUNT Magna Ease valves.
Follow the link below for the latest research in aortic valve replacement.
Click here to access the full publication
For professional use. For a listing of indications, contraindications, precautions, warnings, and potential adverse events, please refer to the Instructions for Use (consult eifu.edwards.com where applicable).
Edwards devices placed on the European market meeting the essential requirements referred to in Article 3 of the Medical Device Directive 93/42/EEC bear the CE marking of conformity.
Edwards, Edwards Lifesciences, the stylized E logo, Carpentier-Edwards, Magna, Magna Ease, PERI, PERIMOUNT, and PERIMOUNT Magna are trademarks or service marks of Edwards Lifesciences Corporation or its affiliates. All other trademarks are the property of their respective owners.
Keywords: bioprosthesis; aortic valve replacement; long-term outcomes; reintervention; mortality
Bioprostheses are the most common valve type used for aortic valve replacement (AVR) in the UK. Early structural valve degeneration of 19- to 21-mm Sorin Mitroflow LX valves led the UK Medicine and Healthcare products Regulatory Agency to issue a Medical Device Alert in 2017.
This summary presents key data from a single-centre, retrospective study comparing outcomes for the Mitroflow valve and the Carpentier-Edwards PERIMOUNT Magna valve. Theologou et al. analysed data from 2,608 patients, assessing aortic valve reintervention and mortality rates up to 10 years.
Download below to keep up to date with the latest research in AVR.
Click here to access the full publication
For professional use. For a listing of indications, contraindications, precautions, warnings, and potential adverse events, please refer to the Instructions for Use (consult eifu.edwards.com where applicable).
Edwards devices placed on the European market meet the requirements for bearing the CE marking of conformity.
Edwards, Edwards Lifesciences, the stylized E logo, Carpentier-Edwards, Magna, PERI, PERIMOUNT, and PERIMOUNT Magna are trademarks of Edwards Lifesciences Corporation or its affiliates. All other trademarks or service marks are the property of their respective owners.
Keywords: aortic bioprostheses; aortic valve replacement; structural valve degeneration
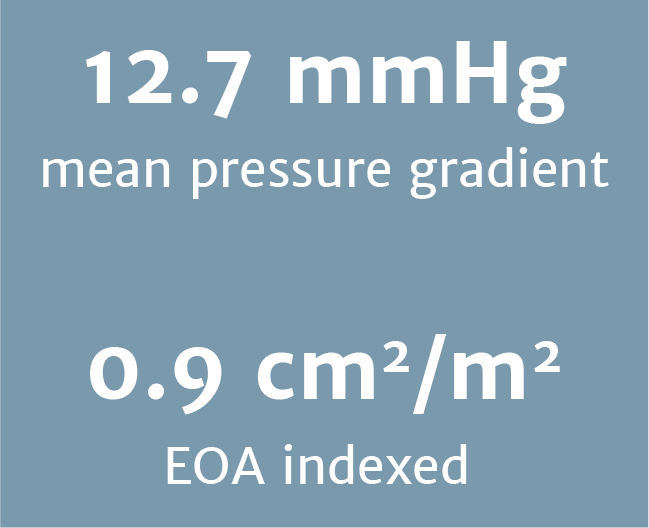
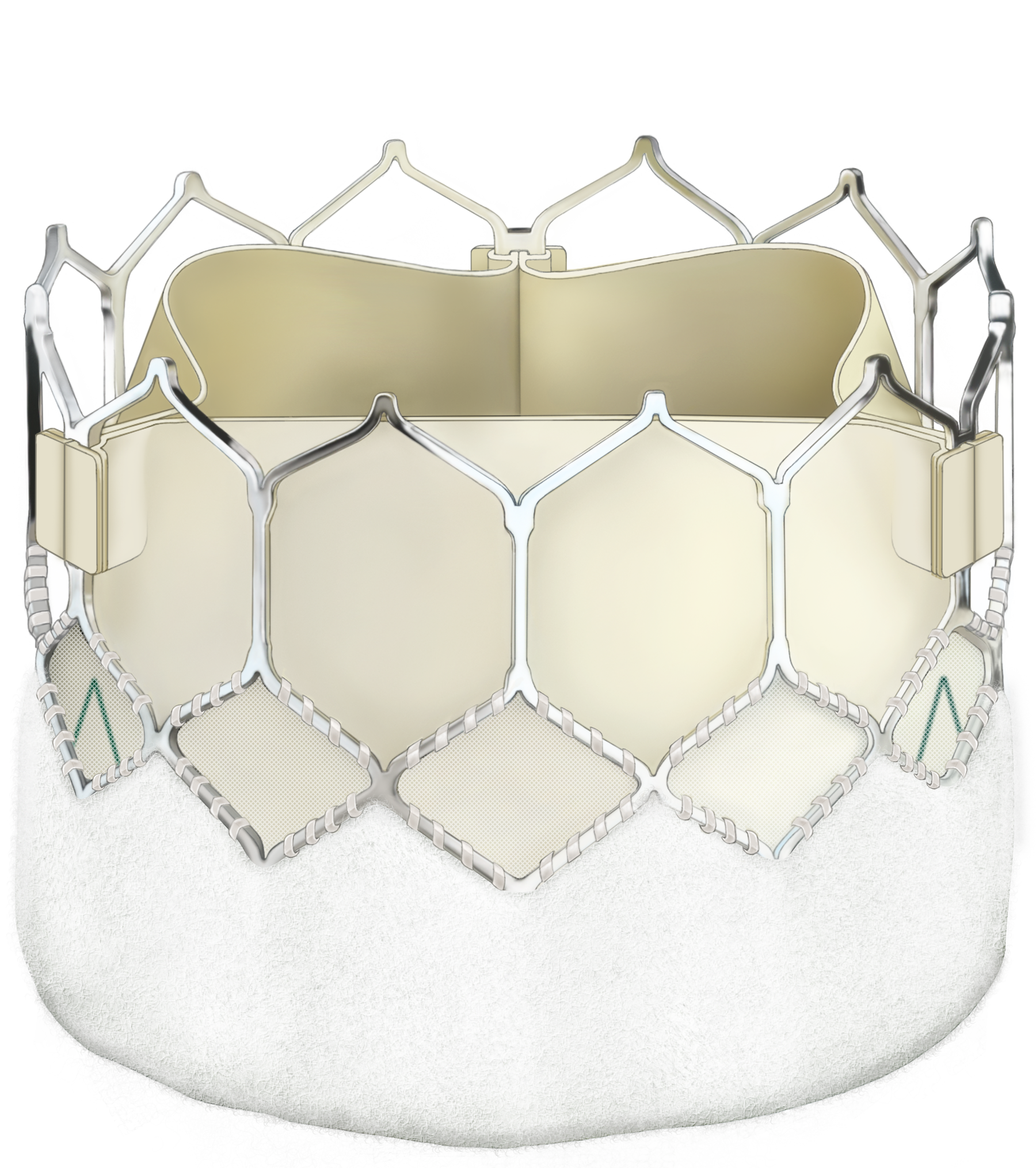
Long-term durability is a key concern for bioprosthetic valves, but measuring structural valve degeneration (SVD) has been complicated by different SVD definitions. The RESILIENCE trial is the first prospective study to use both clinical and imaging SVD definitions to assess long-term valve durability.
This summary describes the design of this multicentre, prospective trial. The trial will investigate predictors of durability and time to failure in RESILIA tissue valves, which are treated to minimise free aldehydes and preserve the tissue.
The trial will include up to 250 adults from up to 15 centres. The primary endpoint is time to valve failure due to SVD, while the secondary endpoints are valve leaflet calcification volume and SVD stage 2 or 3. Non‑contrast computed tomography and transthoracic echocardiography will be carried out at 5, 7, 9 and 11 years after valve implantation to assess valve morphology and haemodynamics.
Download below to keep up to date with the latest research in aortic valve replacement.
Click here to access the full publication
For professional use. For a listing of indications, contraindications, precautions, warnings, and potential adverse events, please refer to the Instructions for Use (consult eifu.edwards.com where applicable).
Edwards devices placed on the European market meet the requirements for bearing the CE marking of conformity.
Edwards, Edwards Lifesciences, the stylized E logo, Carpentier-Edwards, PERI, PERIMOUNT, and RESILIA are trademarks of Edwards Lifesciences Corporation or its affiliates. All other trademarks or service marks are the property of their respective owners.
EACTS Annual Meeting – Lisboa, October 2019